Mit dem Gutscheincode MHK2024 sparst Du die Versandkosten beim Kauf von "Mit Herz und Klarheit"!
Corona – no more dangerous than the flu!?
Author: Herbert Renz-Polster

A great many people are currently putting their hands in the fire for this claim: the new coronavirus is no more dangerous than the flu!
Take a breath and look at the facts
It is high time that we looked at the question in depth: Is the new coronavirus dangerous or not? How does it compare to the well-known influenza?
Instead of clicking through YouTube clips with opinion contributions, you could, for example, take a look at the world yourself. For example, to the places where this virus has spread the most so far. For example to Wuhan, Northern Italy, Spain or New York City. And ask yourself: Why on earth are they making such a fuss – when all they are dealing with is a harmless virus?
But then the answers are already coming, shared a hundred thousand times in the social media: air pollution is to blame, or the many antibiotics that people there take, their immune system is weakened by vaccinations… And anyway: this is all just the result of the panic that is now spreading – no wonder that hyperventilating grandmothers are now storming the intensive care units. So: everything is exaggerated, the result of panic and wrong politics.
New publication on COVID-19
A scientific publication comes at the right time. In the most famous medical journal in the world.
It is timely because this article will be read by those who think COVID-19 is dangerous – as well as by those who think the new coronavirus is safe!
So let’s take a look at it. At a first glance it seems to support the claim that COVID-19 is not really that much of a problem. At least in terms of mortality it does seem to play in the flu league:
If one assumes that the number of asymptomatic or minimally symptomatic cases is several times as high as the number of reported cases, the case fatality rate may be considerably less than 1%. This suggests that the overall clinical consequences of Covid-19 may ultimately be more akin to those of a severe seasonal influenza (which has a case fatality rate of approximately 0.1%) or a pandemic influenza (similar to those in 1957 and 1968) rather than a disease similar to SARS or MERS, which have had case fatality rates of 9 to 10% and 36%, respectively.
So: the mortality rate of COVID-19 is not quite as low as that of the „normal“ flu. But it is far from the dizzying range we know from the other coronavirus-related diseases SARS and MERS (9 to 36% of those affected died from these coronavirus diseases, which occurred pandemically in 2002/2003 and 2012 respectively).
Have those who consider COVID-19 to be a great danger and therefore lock people like you and me in their homes, been wrong?
It gets even more exciting
The second look at the publication is even more fascinating: the article is written by one of the most famous epidemiologists in the world, Prof. Anthony Fauci. Known to many as the small, serious man who face palms when his boss Donald Trump once again talks nonsense.
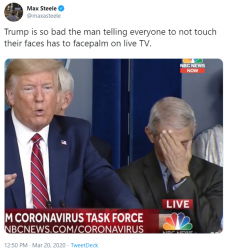
The New York Times calls the little man to the right of Donald Trump „the most vocal advocate of emergency measures against the new virus„: Dr. Anthony Fauci, the director of the U.S. Center for Disease Control.
That the corona sceptics now refer to this man of all people is remarkable. It is similar to how climate skeptics would draw their evidence from a publication by Greta Thunberg. Indeed, Mr Fauci’s authority misses no opportunity to convey to the public the very message that the COVID 19 sceptics reject: Take this virus seriously, be consistent and tenacious in its containment, otherwise a societal disaster will ensue.
And this top scientist is now siding with the „less dangerous than the flu“ faction?
Reading educates
So let’s go through the publication together. Don’t worry, the content is easy to understand, even by laymen (you still need a little more patience than with a YouTube movie).
The article is a so-called editorial. It is a commentary on two „real“ research papers that appear in the same issue (in them, two teams of Chinese scientists describe the previously known characteristics of the new pathogen based on observations and measurements in China). In his commentary, Prof. Fauci summarizes the characteristics of the new pathogen, which are now becoming increasingly clear. In particular, he mentions two characteristics that experts need in order to calculate the course and medical consequences of an epidemic:
- the case fatality rate, which indicates the proportion of people diagnosed with COVID-19 who will eventually die, and
- the infectious potential of the new pathogen, described as the so-called basic reproduction rate. This number indicates the average number of people an infected person will infect if there is no immunity in the population.
How misunderstandings emerge
In fact, Dr. Fauci gives a case-specific mortality rate for SARS-CoV-2 that is lower than many experts initially suspected (this was already indicated by the data from the Chinese provinces outside Huwei).
However, anyone who now thinks that this is why the fear of the new virus is unfounded is unfortunately still wrong. And those who want to prove with this figure that COVID-19 is not worse than the flu are also wrong.
I will explain this as best I can. I promise, no emotions.
In fact, it is good news that COVID-19 mortality is on the whole rather moderate. The health effects on the individual affected (Dr. Fauci speaks of „clinical consequences“) are much less severe in COVID-19 disease than in other pandemic coronaviruses.
However, the health effects of a wave of infection on a population also depend on other influences, with case-related mortality being only one factor, one piece of the puzzle. Yes, the effects on the population also depend on how many infected people die on average when they contract the disease (i.e. case-related mortality), that is correct. But beyond that, the population-related health effects of an epidemic depend on several other factors. These include:
- how many people in total can become infected during the course of the wave of infection
- how quickly people can become infected with the respective virus (this value is important because it helps to determine how many people become ill at the same time)
- how severely people fall ill due to an infection (this value also determines the „disease pressure“, i.e. how much a virus will burden the medical care system)
- how good the medical care of the sick people is, so that they survive an illness as well as possible.
And with these questions – they can be found in standard textbooks on infection epidemiology – we then come to the other figures and data that Prof. Fauci mentions.
Unfortunately, these other influences, which are also important for the course of the epidemic, are not as good as case-related mortality. Here, the new virus causes some concern when compared with the influenza viruses.
The tendency of the new virus to spread
It has been shown that the SARS Co-2 virus spreads much faster than the regular influenza viruses. According to Prof. Fauci, the basic reproduction rate of the new pathogen is considerably higher than that of normal seasonal influenza. While only 1.28 people on average are infected with influenza in one infected person, this is 2.2 people in a SARS-CoV-2 infection. (One reason for this is that, unlike influenza, there is no immune protection against SARS-CoV-2 in the population).
In concrete terms this means that SARS-CoV-2 is spreading – at least imitially – with a much faster snowball effect. And this ensures that significantly more people become ill at the same time. So while a wave of influenza from November to April drives people with severe courses of the disease into clinics, this time frame is „compressed“ to a much shorter period in the case of SARS-CoV-2. If the pathogen runs freely through the population, it can bring more people to the clinics in a few weeks than an influenza can bring in a whole year (the resulting „wave of disease“ is therefore high and narrow). In fact, the basic reproduction rate of SARS-CoV-2, at 2.2, is about as high as that of the Spanish flu of 1918/19.
The infection reservoir
Also with the second point (i.e.: how many people can be infected) things do not look so good for COVID-19. Depending on the country, about 9% – 18% of the population fall ill with influenza every year – but with COVID-19, it must be expected that a much larger proportion can fall ill, namely three to five times as many.
This fact also drives up the number of people who need medical care on a given day, in a given week, in a given month.
The severity of the disease or frequency of complications
Let us then take the second last point: how seriously people fall ill after an infection. This point is perhaps the greatest nastiness: the rate of severe courses or the complication rate is significantly higher with COVID-19 than with influenza! On the one hand, this is due to the pathogen itself, which has a fatal tendency to trigger pneumonia very easily (microbiologists speak of a high virulence). But it is also due to the fact that, in the case of the influenza but not in the case of COVID-19, many people affected are partially protected from severe courses because their immune system is partially prepared (after all immunity is naturally „refreshed“ every few years; in one third of cases, this is also helped by vaccination).
Indeed, severe courses of COVID-19 occur at least 5 times more frequently than with seasonal influenza. This can easily be shown by the data collected so far: In a typical seasonal influenza about 1 – 2 % of the patients have to be treated in hospital, depending on the year. For COVID-19 this is 5 to 10 times more, depending on the population studied so far. This means that if an average 60-year-old (like me) is infected with SARS-CoV-2, the probability that I will fall seriously ill and end up in hospital is many times higher than with a normal seasonal flu. This is also a decisive reason why we are now desperately searching for ventilators and are trying to quickly upgrade the intensive care units in this republic.
And there is another fact I want to mention, which is part of the comparison between COVID-19 and influenza. It is often claimed that COVID-19 is almost exclusively responsible for the death of the elderly and sick. Some people imagine that the tree is shaken and some old leaves fall down. Nothing could be more wrong, because: if one considers the factors that make a more severe course of COVID-19 more likely (age, disease, immune status), these factors apply to about one third of the German population. That would be many leaves. In addition, this must be said with regard to the data: The fact that „only the old and sick“ are affected is neither true for COVID-19 nor for influenza. But it is true for COVID-19 even less than for influenza. According to the latest figures from the US CDC, 36% of the citizens treated in hospital for COVID-19 belong to the 65-84 age group, 17% to the 55-64 age group, 18% to the 45-54 age group, and 20% were between 20 and 44 years old. So much for „only the old“…
This means that, due to the rapid snowball effect on the one hand and the very high medical treatment needs on the other, a COVID 19 epidemic will exceed the carrying capacity of the health care system much faster than an influenza epidemic.
And this is the schizophrenic face of the epidemic: despite the theoretically rather „benign“ mortality, a COVID-19 epidemic can quickly result in more patients per day/week/month than even a good medical system can treat.
Comparisons of figures must be interpreted with care
And that is also the reason why the often heard numerical comparisons lead into no man’s land: Yes, in one flu season in Germany between 500 and 20,000 people die each year, depending on the severity of the disease. The total mortality rate per year increases by 0.05 to 2% as a result – in other words, sometimes a low excess mortality rate, sometimes a higher one. But the rule of thumb is always: these patients die spread over many months. Of course, the healthcare system is also under great strain. Only: the mortality measured in a given week increases as a result perhaps once by 30%, perhaps also once by 50%. However, if the COVID-19 wave is poorly braked – as the data from Italy show – the mortality measured at a certain point in time can increase rapidly by 700%, i.e. by a factor of 7. With an unchecked COVID-19 wave, it can increase even more (whoever likes and has an affinity to statistical models can simulate such influences here)
And this is also the reason why population-based number games do not help us much in the question of dangerousness: Yes, according to the WHO, up to 650,000 people worldwide die of influenza every year. And yes, so far only perhaps 50,000 have died of COVID-19 (as of April 1, 2020, in a week there will be twice as many, etc.). But we are at the beginning of a pandemic that so far has only been raging really hard in small, regional pockets of the world. Its peak is not expected until May or June for most parts of the world. In many areas it has either not yet really arrived or it has been slowed down by clever, responsible action by political leaders. If you can do a little math, you can calculate what an unchecked global passage of this epidemic would mean (or use a pandemic simulator).
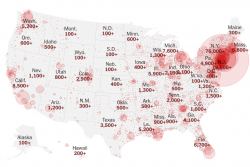

The two maps show this: So far this pandemic is not yet a wildfire. We are at the beginning of the pandemic, the points marked will spread. Whoever refers to current data relating to large areas (such as Euro-MOMO) to point out the harmlessness of this epidemic should take another look in 4 to 8 weeks. The epidemic will be mapped out. If we are lucky and act wisely, it will be less visible than if we fail to do both.
The reference to baseline mortality also leads into no man’s land. Yes, in Italy 600 000 people die every year, that is 1600 people a day. And now, instead, it is about 2600 a day. Is it bad? Yes, it’s bad. Such figures are no cause for alarm, they should be seen as a warning. They show how dangerous this virus can be. After all, over 60% of the 1,000 additional deaths in Italy come from Lombardy, which is home to only 10% of the Italian population. If all areas of Italy had been similarly affected, not 2500 people would have died today, but perhaps 6000 – that is 4400 more than normal. THIS overburdens every health system.
Vicious circles
But that is not enough. The characteristics of SARS-CoV-2 as described above can create vicious circles, which in turn can lead to a less favourable course of the epidemic.
And this brings us back to the case-related mortality describes above, which regarded in isolation is not so frightening. Right from the start, the data on reported mortality were clear: in one place on earth (e.g. Wuhan/China) up to 20% of symptomatically ill people have died. In the other Chinese provinces, however, only 0.7% died a few weeks later. The situation is similar in Italy, where the mortality rate was (and still is) significantly higher in the severely affected areas than in the less affected areas. Yes, one can almost see a linear correlation: The more affected an area/province/country is by this epidemic – the higher the case-related mortality of COVID-19 increases! Hence the reference to the „all in all taken together“ at the beginning of this article: Even if the textbook will say that COVID-19 has a case-related mortality of 0.X percent, it may have a completely different, partly frighteningly higher mortality in the country XY in calendar week XY.
The resulting vicious circles should not be underestimated: Depending on the quality of the healthcare system and its current performance, the de facto mortality rate for COVID-19 can exceed the theoretical mortality rate by a factor of 30 to 50.
This sharp increase is partly – unfortunately – also explained by an extremely undesirable reinforcing effect: If a health care system collapses under the burden of those to be cared for, the inevitable backlog not only affects those who are ill with COVID-19 – but also the other patients who are dependent on good medical care: Heart patients, children with seizures, newborns with a (in itself easily treatable) newborn infection, people with allergic reactions who perhaps only needed an injection of adrenaline, and so on.
This is another reason why there is a desperate search for a strategy to control the epidemic so that our health system does not collapse under the burden.

There is a reason why you don’t need to read such headlines during a normal flu epidemic: despite a roughly similar case-related mortality rate, COVID-19 plays in a completely different league than influenza in its episodes.
To sum up
So, to sum up: The problem with COVID-19 is that, because of the rapid snowball effect, the fairly high complication rate and the resulting high need for medical treatment, the epidemic exceeds the carrying capacity of the health care system much faster than even a full-blown wave of influenza.
And that is precisely why, despite its similar theoretical mortality, we have NO need to order additional respirators for seasonal flu, nor do we see floating military hospitals in New York City Harbor – nor do we have to endure a „lockdown“ of society.
Therefore, the question of how many deaths will be caused by COVID-19 is also pointless. The above shows one thing: this does NOT (or only to a small extent) depend on the theoretical mortality rate – but mainly on how well we manage to control this epidemic, so that, for example, people do not compete for treatment or even respiratory care, as is currently the case in New York (and will certainly happen in many places around the world).
I really hope these considerations will also come up also at the „vertigo-ambulances“ of this republic.
The death
In order for them to do so, I will end by talking about something else that distinguishes the influenza virus from SARS-CoV-2. It’s the way of death. I hate to talk about it, but I still think it’s important. It is also important in order to understand why the health workers fighting this epidemic in overworked hospitals are so often traumatised and will carry their efforts with them for the rest of their lives. It is also important because all the nonsense parroted in this debate will only fade away when people are able to face the facts as they are. It is easy to talk if you do not open your visor.
The SARS-CoV-2 virus has a few nice features (such as not really being interested in children, and also that pregnant women, for all we know, have rather little to fear – we can’t celebrate it enough).
But this new virus also has a very tricky feature – it attacks the lungs very easily. In fact, even with less severe courses, opacities can regularly be detected in the lungs. Now the immune system can usually deal with it and prevent the progression to severe, diffuse pneumonia. But sometimes it cannot. To be more precise: Much more frequently than with influenza not! This is the reason why many people affected by COVID-19 need ventilation at least temporarily in order to get well again – in the case of influenza this is only in exceptional cases. The fact is: Of those admitted to hospital because of COVID-19, about 30 to 75% need intensive medical care, depending on the country and health system. Half of them need artificial respiration.
And really people: Well, if they do get one (and the ventilator may not be occupied because our Minister of Health followed the advice of „COVID-skeptics“ to just let this epidemic go). Because what comes now is serious: Death from diffuse pneumonia is different from death from heart attack or circulatory arrest or simply from old age. It is not a gentle death. All doctors (including myself) who once sat at the bed of a patient who had to die from insufficient breathing, i.e. from lack of oxygen and hyperacidity of the blood, know what that means. And above all: how much help such a patient needs to go this way. Well, if this help can be given.
We must do everything possible to ensure that this help is then also available. In other words: We must also therefore spread the epidemic as best we can, please do not be seduced.
This text was translated by DeepL. Please comment for corrections.
 Noch keine Kommentare
Noch keine Kommentare
 Kommentar verfassen
Kommentar verfassen 




 Quellen
Quellen





